25 years ago I was rummaging around my teachers desk at the clinic and I saw a two-foot pile of photocopy pages. The top page said LYME DISEASE. I paid no attention to it. Little did I know my teacher thought she had it and she does.
Now Lyme disease is a controversial topic in some corners of medicine. I am just putting this up for information and the “break through” on Lyme is likely years away from accessible treatment. But it’s something to keep an eye on.
Today she, my teacher, says Lyme for her is like a warning light. When she gets over tired, hungry…. it flares and she has to bring her activities back to a more moderate level. It is one of the very few things she says she can not cure. It can be managed but so far… but there is hope.
A new science experiment has shown Lyme bacterium is susceptible to a alteration of it’s manganese levels. Which can lead to treatments to wipe it out. But first lets have a short history lesson.
1. Long before anyone named it
- The bacteria and ticks behind Lyme disease have been around for thousands of years.
- Borrelia DNA has been found in a 5,300-year-old mummy (“Ötzi the Iceman”) and in preserved ticks and mammals from the 1800s. Wikipedia
2. Early medical clues (late 1800s–1960s)
- 1880s–1900s (Europe): Doctors describe strange skin problems and a ring-shaped rash after tick bites:
- 1883: Alfred Buchwald describes a chronic skin condition we now know is Borrelia-related.
- 1909: Arvid Afzelius presents the classic erythema migrans (“bull’s-eye” rash) after a tick bite. Wikipedia
- Mid-1900s: European doctors link tick bites, that rash, and later neurological symptoms (meningitis, nerve pain). Wikipedia
Nobody’s calling it “Lyme disease” yet; it’s just scattered syndromes.
3. The Connecticut cluster and the name “Lyme” (1970s)
- 1975 – Old Lyme & Lyme, Connecticut: Parents notice many kids with a weird arthritis that looks like juvenile rheumatoid arthritis. They call health officials. CT.gov
- Yale and CDC researchers investigate and realize:
- The cases cluster near wooded, tick-heavy areas.
- Many patients recall a prior rash.
- By the late 1970s, this cluster is recognized as a new tick-borne illness, named “Lyme disease” after the town. CDC Why now? The theory is people living near a dense, deer infested woods. Ie Bad luck.
4. Finding the actual germ (early 1980s)
- 1981–1982: Medical entomologist Willy Burgdorfer isolates a spiral-shaped bacterium from deer ticks and then from patients with the disease. NIH Intramural Research Program
- The organism is named Borrelia burgdorferi after him.
- Once it’s known to be a bacterium, Lyme becomes treatable with antibiotics, and research explodes.
5. From local oddity to major public-health issue (1990s–today)
- Since the 1980s, Lyme disease has spread and been recognized more widely in North America and Europe, especially as deer and tick populations expand and forests regrow. Yale School of Medicine
- It’s now the most common vector-borne disease in the U.S., with hundreds of thousands of diagnoses per year. Johns Hopkins Lyme Research
I have loosely followed Lyme for years, but when I have a patient with it I always suggest they see my teacher as it seems very difficult and involved to treat unless detected early and the correct Western drug therapy’s are used. She has personal and professional experience so it’s best to go there.
But from my exposure to it. It seems very hard to diagnose in a clear manner and equally complex to treat. I have seen simple antibiotics if used early enough. But I have had a patient that came and said the ER doctor threw the tick in the trash saying there is no Lyme here and no testing was done.
CityNews / NEWS 1130 (Nov 7, 2016)
- “New bacteria that causes illness similar to Lyme disease found in BC ticks” — reports three BC ticks tested positive for a Borrelia mayonii–like bacterium. CityNews Vancouver
- Important: No human cases from that new bacterium were confirmed in BC at the time. picnet.ca
BCMJ Clinical Article (June 2011)
- “Lyme disease in British Columbia: Are we really missing an epidemic?” by Bonnie Henry & Muhammad Morshed. bcmj.org
- The article explicitly states there was no evidence for a Lyme disease epidemic in BC: they point out low tick infection rates (< 1%) and very low human case rates. bcmj.org and it clearly acknowledges Lyme is real.
PICNet / BCCDC Release (Nov 7, 2016)
- “Lab testing confirms new Lyme‑related bacteria discovered in three BC ticks” — same as the CityNews story, from a health‑authority source. picnet.ca
The BCMJ article notice the authors.
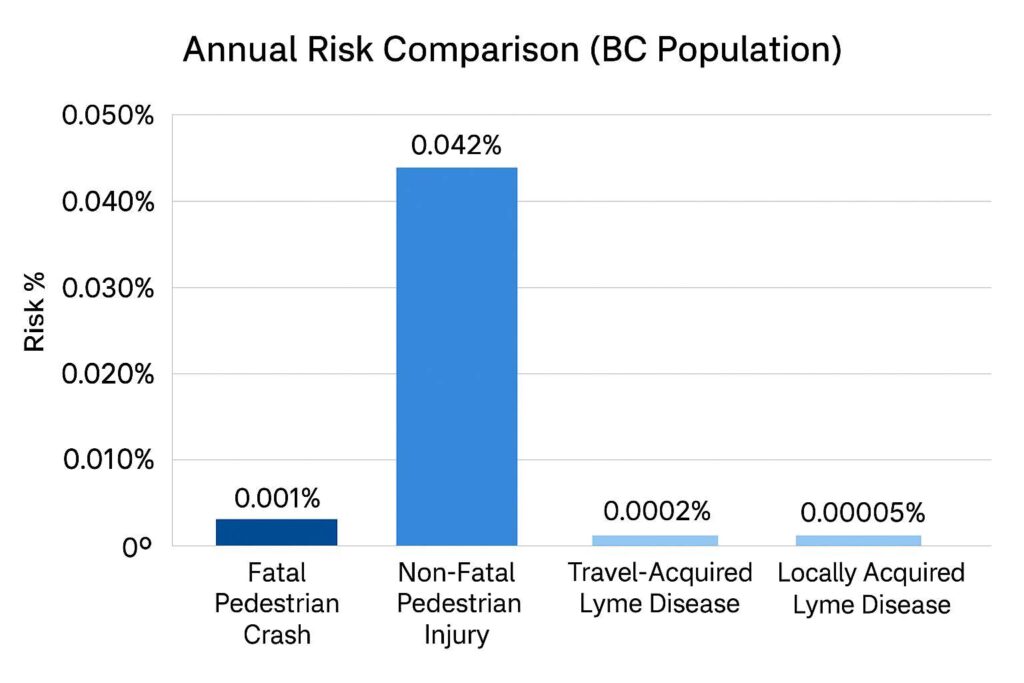
This chart I got from here It is quite reassuring actually as you are way more likely to be hit by a car (see below) than get Lyme. I absolutely know that for people that have Lyme it really sucks. Once it is established it can ruin and kill the person, and that is why I keep an eye on the treatments for Lyme. I do not want to minimize the chances of getting it or the seriousness for people that have it.
This BC site has several interesting Lyme articles.
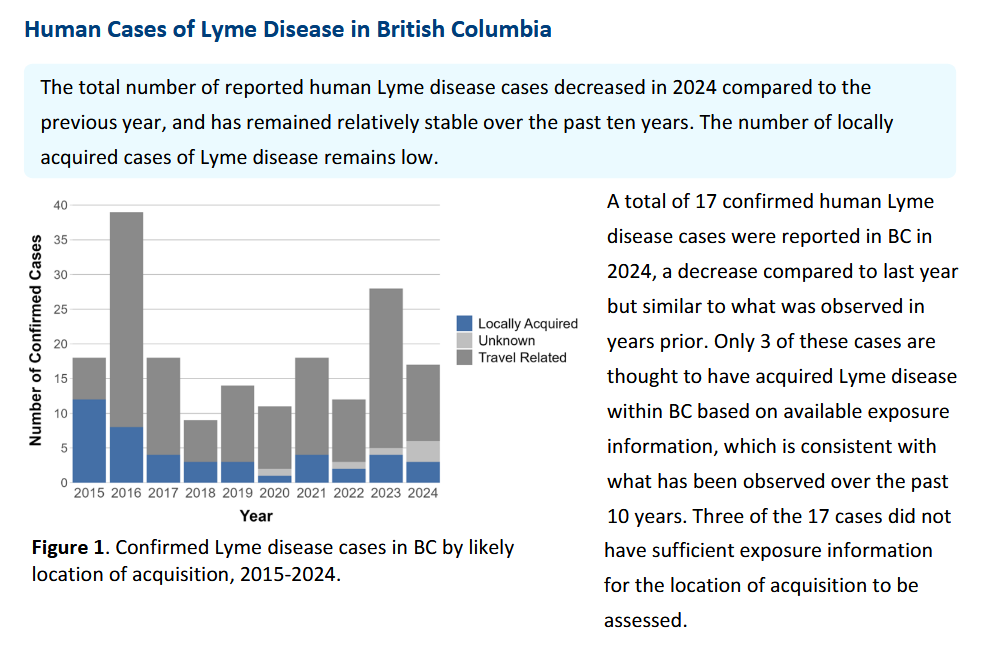
All levels of Governments acknowledge there is Lyme. The confirmed cases in BC certainly do not line up with the amount of people who feel they have it. But I imagine low level auto-immune illness will have a lot of overlap with symptoms and the lack of simple, conclusive testing can lead people to land on a certain ailments.
Just to show the world does agree that Lyme exists as for real it was hotly debated 20 years ago. Maybe the amount of actual cases was debated.
| Organization | Lyme Disease Recognition | Prevalence / Endemic Areas | Key Guidance / Note |
|---|
| WHO (World Health Organization) | Recognizes Lyme borreliosis as a tick-borne disease caused by Borrelia burgdorferi | Mainly North America, Europe, parts of Asia | Prevention through tick bite avoidance, early diagnosis, and treatment; provides global fact sheets |
| CDC (USA) | Recognizes Lyme disease; tracks annually | ~300,000 cases per year in the US; endemic in Northeast, Upper Midwest, parts of Pacific Coast | Maps risk areas, provides testing protocols, tick prevention guidelines, case definitions |
| PHAC (Canada) | Recognizes Lyme disease; reports both travel-acquired and locally acquired cases | Endemic in southern BC, southern Ontario, southern Quebec, parts of Atlantic provinces | Surveillance, prevention, awareness campaigns, testing guidance |
| BCCDC (British Columbia) | Monitors Lyme disease; distinguishes travel vs locally acquired | Southern BC; locally acquired cases are rare but rising | Tick bite prevention, diagnostic info, reporting, public education on local risk areas |
All this to say the recent peer reviewed research says (whole article here – Science paper here)
Northwestern and USU researchers found a new weakness in the Lyme bacterium Borrelia burgdorferi that all revolves around manganese:
- The bacterium uses manganese as part of a two-layer defense system:
- An enzyme (MnSOD) that acts like a shield against destructive oxygen radicals.
- A pool of manganese-containing metabolites that act like a sponge, soaking up any radicals that get through. Northwestern Now
- Using advanced techniques (EPR imaging and ENDOR spectroscopy), they made a molecular map of how manganese is stored and moved inside living B. burgdorferi. Northwestern Now
- They discovered manganese is a “double-edged sword”:
- If the bacterium is starved of manganese, it loses these defenses and becomes vulnerable.
- As the bacteria age, their “sponge” pool shrinks; at that point too much manganese becomes toxic because they can’t safely store it anymore. Northwestern Now
- This suggests several new drug strategies:
- Starve B. burgdorferi of manganese.
- Disrupt its manganese complexes so the shield/sponge can’t form.
- Or overload it with manganese once it can no longer buffer the excess—pushing it into toxic stress. Northwestern Now
Big picture: the study identifies manganese handling as an Achilles’ heel of the Lyme bacterium, potentially opening a path to treatments that don’t rely solely on long antibiotic courses and instead make the bug more vulnerable to the body’s immune system.
unfortunately
A treatment from this discovery is likely many years away, if it happens at all.
What this study actually is:
- It’s basic mechanistic research in bacteria and model systems, not a drug trial. It shows that Borrelia burgdorferi has a manganese-handling weakness that could be exploited, but it does not test a specific drug in humans. bioquicknews.com
- Steps between this and a real treatment (best-case pipeline):
- Identify or design molecules that:
- Starve the bacteria of manganese, orDisrupt its manganese “shield/sponge,” orOverload it in a controlled way.
- Test tubes / cultured bacteria.Animal models (e.g., infected mice).
- Identify or design molecules that:
- What the article does not say:
- There is no mention of a candidate drug in clinical testing.
- No announced start of human trials.
- No projected therapeutic product or date. bioquicknews.com
Given that, any specific date (like “5 years”) would be made up. Realistically:
- If everything went unusually well, you’re looking at a multi-year arc from discovery → candidate → trials → approval.
- It’s also completely possible this mechanism ends up as “just” important biology that informs better use of existing antibiotics or combination therapies, rather than its own drug.
If you want something actionable now, I’d focus on:
- Optimizing current guideline-based treatment for acute Lyme. Patient side – Professional side
- Symptom-focused, multidisciplinary care for persistent symptoms. I can tell you from over 100 conversations with Lyme people there is more Snake oil sold to treat Lyme than useful stuff. From my little research for this section on adjunct treatments for Lyme, even I was shocked at some of the BS (bad stuff) sold saying it will help. I can tell you Lyme can be incredibly tough to treat. If the practitioner thinks differently, run.
- Keeping an eye on this line of research for when they move from mechanism → animal models → early human trials.
I read quite a bit of medical reviews for sure 5-10 a week. I am always stunned at the space between “discovery” and you can actually go buy it. There is one on repairing tooth enamel from Keratin from sheep wool. Supposed to be for sale by 2028. We’ll see…
If you have Lyme, I am sorry. It sucks.
There is help, there are people in a variety of fields that have ways to help. The trouble is, like all weird illnesses, they don’t always work on everyone or anyone. But you need to keep looking, asking, thinking, learning. My teacher is a great resource. She has hers under control, most of the time. Which again tells me how difficult it is to currently cure it. As she’s smarter than most.
Keep looking, keep asking, keep thinking and when it makes sense. Try it.
Be Well,
Ward Willison R.Ac.
allbodycare.com
Kelowna Acupuncture & Other Natural Therapies